2016 Miracle Kid Joshua Sanchez

It was a night like many others for Melissa Yeager and her son Joshua Sanchez at the Bloomsburg County Fair. They’d been walking around, enjoying the fair and teasing one another while waiting for a special guest to come on stage.
“Josh was 14 and I thought it would be funny to see Barney,” Melissa said with a laugh. “He was complaining about being hungry, and I told him, ‘Not until we see Barney.’”
They stood in front of the stage waiting for the big purple dinosaur, but the joking subsided when Ms. Yeager looked over and saw an all-too-familiar look on Joshua’s face. She quickly grabbed Joshua, wrapping him with her body and falling to the ground, allowing Joshua to safely fall on top of her so he would not be hurt.
This was a familiar scene for Joshua and his mother while he was living with epilepsy.
“I started having seizures when I was 4 months old. They got worse year by year and I started having more and more,” Joshua said.
The first seizure Joshua experienced was a febrile seizure, or a convulsion caused by a high fever. Febrile seizures are relatively common, but in rare cases scarring from a prolonged seizure can have long-term effects on some children, according to Jill Gotoff, M.D., pediatric neurologist at Geisinger Janet Weis Children’s Hospital.
Over the years, the frequency of Joshua’s seizures varied depending on which medications he was taking. When one medication stopped working, he would be prescribed higher doses or switch to other medications.
“I could have seizures as often as a few times a day,” he said. “I was limited in what I was able to do because of the fear of having a seizure.”
Joshua had some horrible seizures. Once he fell and hit his face on of a table. Another happened while he was walking down the street. He had several while playing with neighborhood friends. Joshua remembers one particular time in school.
“I was in sixth or seventh grade, and I remember coming back to class after visiting the nurse to everyone in class crying and really upset,” he said. “It scared everyone that time.”
For his mother, each time was scary.
“I would take him to the hospital every time he had a seizure. The Geisinger doctors finally suggested that I didn’t have to take him unless the seizure lasted more than 5 minutes,” Melissa said. “They said if it was more than 12 minutes and the ambulance was not there, that I needed to get him there by car, because if he stopped breathing for that long, it could cause lasting damage.”
Melissa continued to be as protective of Joshua as possible.
“We loosened the screws on his bed, so I could hear him moving,” she said.
“If I would move an inch she would say, ‘Josh, are you OK?,’” Joshua joked.
At age 14, Joshua’s seizures were still quite frequent. His mother called Linda Famiglio, MD, pediatric neurologist, to let her know of recurrent seizures and ask if his medicine might need to be adjusted. Dr. Famiglio recommended that Joshua see Dr. Gotoff to determine if he was a candidate for surgery.
“I saw Joshua for the first time in 2014, and we began the evaluation for surgical candidacy, which included imaging studies, EEG testing and reviewing his medical history in detail,” Dr. Gotoff said. “At the time that I saw him, he was looking at potentially never being able to have a driver’s license if he continued with his seizures. So it was an opportune time to consider more aggressive management.”
With epilepsy, doctors are extremely cautious about recommending a patient for surgery by ensuring that all appropriate medical options are explored while waiting to see if the child will outgrow the seizures.
“A majority of children will grow out of their seizures in their teen years,” Dr. Gotoff said. “There is a tipping point, where you know they are not going to outgrow them — and then it is a matter of being as aggressive as you can or as aggressive as the families are ready to be.”
Joshua and his mother were ready to pursue aggressive treatment and began months of testing to determine the exact location in his brain that was causing the seizures.
“They did many different tests. They shot dye followed by medication up to one part of my brain through a catheter and had me do things like count down from 20. When they put the dye on my left side, I would say 20 and then my voice would trail off,” Joshua said. “It showed that I needed the left side of my brain to control my speech and I was lucky since the right side was where the seizures were coming from.”
The testing began with the long-term monitoring with the EEG. Joshua had electrodes placed all over his scalp. This test showed that he had more right temporal discharges but also showed some left-sided spikes as well. This indicated that the seizures were most likely coming from his right side, but there were still much more testing to do.
After the EEG, Joshua had MRIs and extensive neuropsychological testing that took many hours to assess all parts of his brain for areas of strengths and weaknesses. Joshua had a PET scan, which is a radiologic test that shows how the brain metabolizes glucose energy. The PET scan showed decreased and abnormal metabolic activity in Joshua’s right temporal lobe.
“It is kind of like trying to put all of the pieces of a puzzle together,” Dr. Gotoff said. “We saw evidence of a lesion on the right temporal part of the brain, and most of the pieces of the puzzle were pointing to that area, but we still needed to be as accurate as possible.”
The final part of the evaluation — and the most invasive — was to surgically implant electrodes directly over the brain surface. Doctors removed a large part of Joshua’s skull in order to place a grid of electrodes on the surface of his brain, monitoring him for several days.
“The electrodes sit on the brain surface recording underlying EEG activity while the other side is connected to an EEG machine,” said Amir Kershenovich, M.D. pediatric neurosurgeon who performed the procedure. “This allows us to monitor the electric activity of the brain and directly record it, as opposed to the typical EEG which are done through the scalp. This gives us more accurate information.”
“I had a week of lying in bed with wires coming out of my head. They took me off the medicine to allow me to have seizures while they monitored,” Joshua said. “This let them get a good reading of where the seizures were coming from.”
The other advantage of placing the electrodes directly on Joshua’s brain was that it allowed Dr. Gotoff to access the function of this part of his brain.
“I was able to stimulate each of the contacts on the grid and do what we call mapping,” Dr. Gotoff said. “For instance, I might see that contacts 3 and 4 could be where his seizures are coming from, but contacts 5 and 6 are where he has sensation of his tongue or maybe movement of his hand. We have a general idea of where those functions are, but it is different for every person.”
The grid allowed the doctors to map Joshua’s brain function and his seizures and make sure there was no significant overlap. This gave Dr. Kershenovich a clear picture of what could be safely removed and which areas controlled important functions.
“In brain surgery, we remove as much as we can and what is can be safely removed,” Dr. Kershenovich said. “We want to be as thorough as we can, but we want to be as conservative as possible as well. There is always a possibility of going back to take additional parts out, but there isn’t a possibility of putting anything back.”
After a week of monitoring and testing, Dr. Gotoff and Dr. Kershenovich located the exact spot of the seizures in the right temporal lobe. They determined that the section could be safely removed without causing any harm to Joshua.
The second surgery involved removing the electrodes – as well as the part of the brain that was the source of the seizures. The surgery lasted 11 hours; the doctors removed about 8 percent of Joshua’s brain.
Joshua had two seizures after returning home.
“Dr. K explained that if the seizures are in there, they must have to come out,” Joshua said.
Since September 2014, Joshua has been seizure-free — the longest period of time that he has been seizure free in his entire life. He still takes some medication but not nearly as much as he did before. The plan is to wean him off medication as time goes by.
“So far he has been more than one year seizure free,” Dr. Kershenovich said. “With the correlations that we had for him where everything pointed to that part of the brain and a successful surgery, his chances of being free of seizures is about 70 to 80 percent.”
For Joshua and his mother, the surgery has been nothing short of life-changing. Joshua recently got his driver’s permit.
“Yes, he is able to drive now. Against my judgement, but Dr. Gotoff said ‘It might be time to let him drive if he wants and to stop babying him,’” Melissa said.
Joshua didn’t let seizures slow him down before and he is not about to slow down now without them. He missed a total of 72 days of school during the testing and surgery and was still able to maintain A’s and B’s in his high school courses.
“I did my work in the hospital, sometimes with only one eye open,” he said.
Joshua is working hard in school and is involved with many extracurricular activities. He has been in the school chorus since kindergarten. He helps his eighth-grade science teacher teach Cub Scouts, is an active member of the Future Business Leaders of America and is involved with student council. He plans to run for council president at the end of this year. He also works a part-time job at Giant.
“Oh, and he also is teaching himself to play the piano,” Melissa said.
Josh plans to attend college and would like to be a pediatric surgeon.
“I’m not sure what type, but I’m thinking about being a cardiovascular surgeon,” he said. “So I’m planning on years upon years of school.”
For now, he and his mom are enjoying their new life.
“It has been life changing,” Melissa said. “I still wake him up in the morning and ask him if he is ok and if he slept ok. I’m working on being less protective and letting let him do more. He is a strong kid.”
Dr. Gotoff is happy with Josh’s progress and feels good about his chances of remaining seizure-free.
“Joshua exemplifies the great success we have had with our epilepsy surgery program,” she said. “Every step along the way, he and his family were very enthusiastic and supportive. His story is essentially what we would like everybody with seizures to experience.”
Dr. Kershenovich sums up what makes Josh a miracle quite simply.
“He’s seizure-free,” he says with a smile.
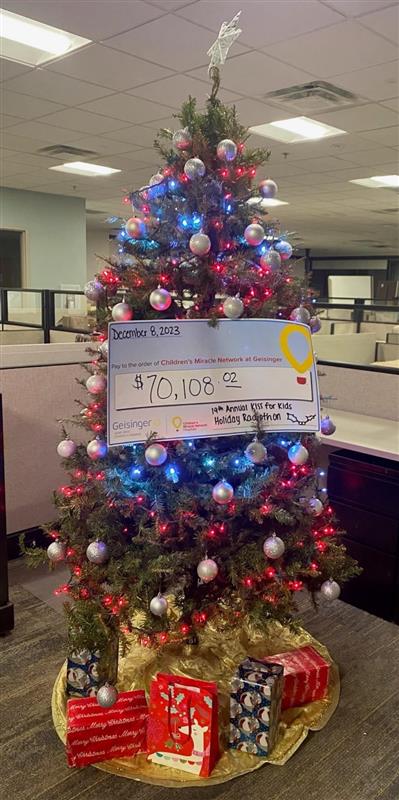
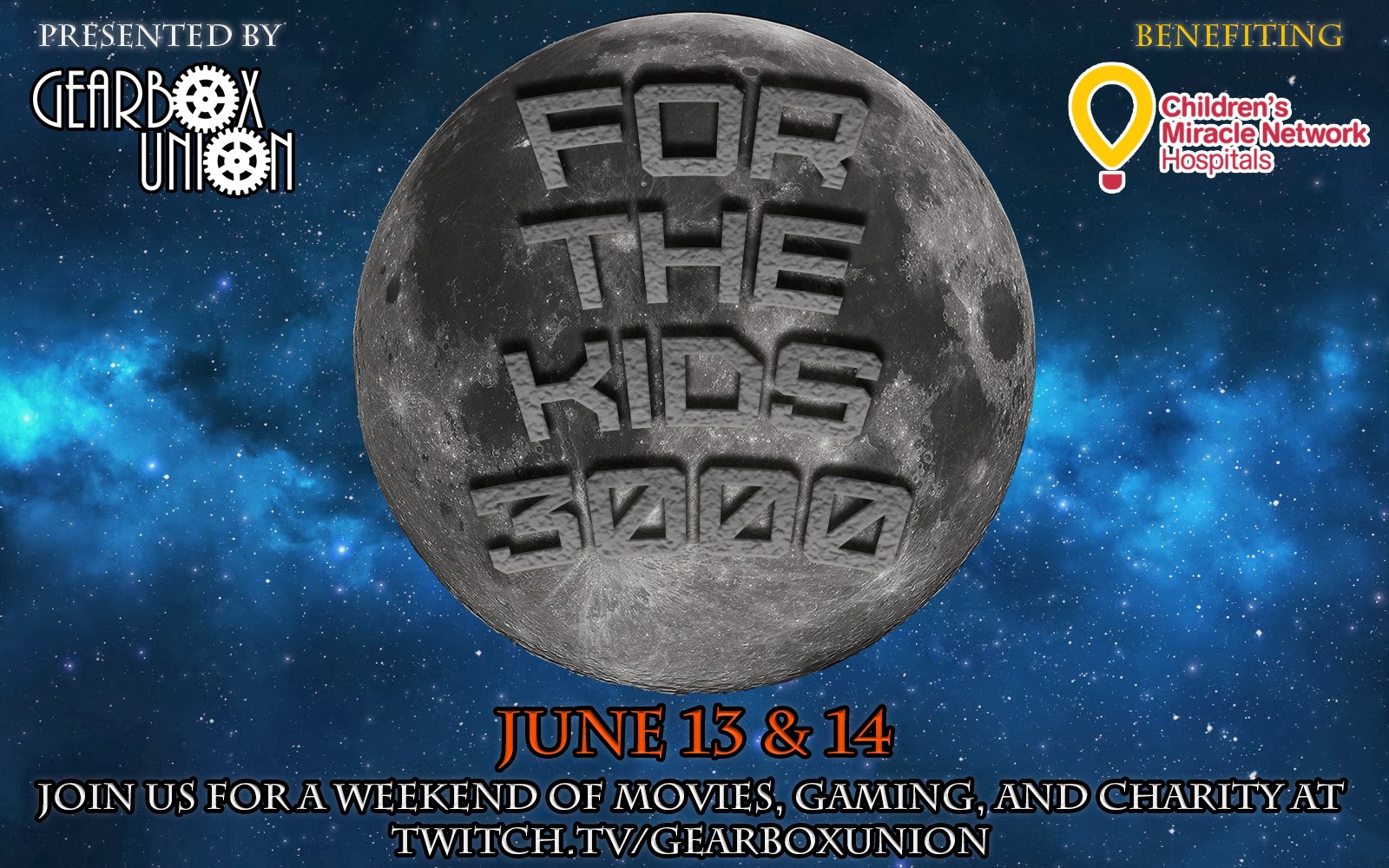
Epilepsy monitoring equipment has been purchased with funds from Children’s Miracle Network at Geisinger. The new monitoring equipment allows kids who are in for long-term monitoring to leave the room and use the playroom at Geisinger Janet Weis Children’s Hospital. Donations also support the Child Life Department, which provides distractions and activities for children who have long stays in the hospital. Many children with epilepsy have attended epilepsy camp at Camp Victory, also supported with Children’s Miracle Network at Geisinger funds.