2017 Miracle family benefits from donations

The Goodman siblings of Vestal, N.Y., are full of character. Grace, Reece and Clark, 11, can easily take over a room with their quick wit and outgoing personalities. They feed off one another and know each other better than anyone.
Perhaps that comes from spending their entire lives together, attending school together and being a close-knit family — or maybe it’s the relationship they built during their fight to live after being born extremely premature, at just 25 weeks.
Amy and Bryan were having trouble conceiving. After visiting a fertility specialist at Geisinger Medical Center in Danville, Amy was given medication to help her ovulate. Not long after, the couple found out the medicine had worked but maybe too well.
“I went the first time, and the doctors said I was pregnant. We went a second time, and they said it was twins. We went a third time, and they said, ‘Uh-oh, there are four,’” Amy said. “I cried and Bryan was in shock. I was not planning to have four and they were all fraternal. The doctor said he never had that happen in his 25-year career.”
After overcoming the shock of having four children at once, Amy and Bryan began preparing for their new family. Things were going well, until 23 weeks into the pregnancy. During a routine exam, doctors noticed that Amy’s cervix was shortened. They were concerned she was at risk for a preterm delivery. She was admitted to Geisinger Medical Center in Danville and put on medications to try to delay the delivery.
Amy lasted a little more than a week until she dilated five centimeters and the doctors realized they were going to have to make a plan for delivery.
“The doctors gave me statistics about giving birth to four. Because of the prematurity, they said they probably all wouldn’t survive and the babies wouldn’t cry and they wouldn’t have their eyes open,” Amy said. “So that was emotionally overwhelming, trying to factor that all in when I just wanted to keep these babies in longer.”
The delivery was planned for Jan. 12, 2006, in the operating room next to the Neonatal Intensive Care Unit (NICU), where the children would be passed through a window to the hands of neonatologists in the NICU immediately after delivery.
“So, we were passed through the window like chicken nuggets?” Clark said as his mother told the story.
“You guys did look like nuggets – shriveled-up ones,” Amy remembered.
“We knew that each of them was going to need breathing tubes, and they were going to need treatment with surfactant, which is a medicine that helps open the lungs and decreases damage from being dependent on the ventilator,” said Lauren Robbins-Johnson, MD, neonatologist at Geisinger Janet Weis Children’s Hospital. “It was all hands on deck with each attending physician dedicated to a baby.”
The first baby born was Sophia, at 1 pound, 8 ounces. Next was Grace, at 1 pound 10 ounces, then Reece, at 1 pound 12 ounces, and finally – Clark, at 1 pound, 14 ounces. Now the fight began for each of them to overcome their extreme prematurity.
“Sophia cried at birth and opened her eyes,” Amy said. “She was the only one that cried and her eyes were open. So she was my hope.”
Because she needed to recover from the surgery, Amy was not able to see the babies in the NICU right away, but Bryan remembers his first visit very well.
“It didn’t look good,” he said. “When they were that small, every time they would breathe, their chests would completely concave. I didn’t know if that was normal or not, but that first night, I didn’t feel good about it at all, about any of them. Those first couple of days were a blur, because you didn’t feel good about anything. Their color was a dark pink. They still had fur, basically.”
“Bryan is right. Their time in the NICU was a blur,” Amy said. “We relied on humor, that was one way to get through the pain of it all. Faith was another big factor, and we had outstanding community support.”
Each child had his or her own personal journey in the NICU — and each had his or her own battle.
The first time Amy was able to see them, she needed to be wheeled into the NICU on her gurney, because she was still recovering from surgery.
“Bryan wheeled me to each of their beds. They couldn’t have them all in one room because they needed to be watched very closely and the nurses usually had two babies at a time,” she said. “The first 48 hours was very much in the balance. Grace was suffering the most.”
Sophia also had a rough start. At 2 weeks of age, she developed sepsis with a bloodstream infection and came close to dying. The infection made it difficult to manage her on the ventilator, and her blood pressure dropped significantly.
“Dr. Johnson explained that Sophia’s stomach was bruising and said that was a sign of internal bleeding,” Amy said. “She said, ‘Eventually it is going to go to her brain and her other organs and she won’t be able to breathe on her own.’”
Bryan and Amy held Sophia for the first time and Dr. Johnson placed her back in the incubator, at which point she started to breath on her own.
“I was given another sense of hope. I had this child I was supposed to be watching pass away right now and she was surviving,” Amy said. “They intubated her and kept her alive.”
A little bit later Clark began having serious breathing problems and — at one point — was given last rites. He also had a blood infection that resulted in some bleeding in his brain, but he managed to recover.
While visiting the NICU, the toughest part for Amy was trying to divide up time for each child.
“I didn’t know which of them needed the most attention,” she said. “I pulled aside some of the nurses and asked them to tell me what different things meant on the monitors. Understanding what all the numbers meant gave me some sense of control, because I felt completely out of control. I couldn’t hold them; I could only hold their tiny hands in the incubator.”
During the next month, all four children started getting a little better — to the point that Amy and Bryan could hold them and the NICU staff started giving the kids nicknames.
“One day I had lip gloss on with glitter in it. While I was holding Sophia and kissing her head. I got some glitter in her hair. I said she looked like a little princess,” Amy said. “So the NICU staff gave her the name of ‘Princess Sophia.’
“Grace was ‘Amazing Grace,’ because we wanted her to get through everything she had been through and she had the toughest road from the beginning. Clark, because he had these big huge eyes and was constantly looking around, was ‘Curious Clark.’ And Reece was the dark-haired, dark-skinned and sturdiest of all four and was growing the fastest, so they called him ‘Regal Reece.’”
Because of what Sophia and Clark had gone through and with Grace and Reece continuing to fight, Amy thought they were all going to be OK. However, on March 11, Dr. Johnson told Amy and Bryan to ask close family to come say goodbye to Sophia, because she was not going to make it through the weekend.
“The bloodstream infection she had caused bleeding in her brain and it progressed into pretty severe permanent brain damage,” Dr. Johnson said. “She developed seizures and had areas of her brain that didn’t develop properly.”
“I was confused, because she had just gone through what I thought was a miracle to survive,” Amy said. “Dr. Johnson said the damage was too bad, and she showed me the scan of her brain. There was a lot of black emptiness. Dr. Johnson and I had a really good cry at that moment.”
On March 13, Amy and Bryan spent the entire day by Sophia’s side. Toward the evening, Sophia started to get worse and they asked if they could take her outside to pass away.
“We didn’t want to be in that room where we had already seen other babies die,” Amy explained.
The NICU staff detached Sophia from all the equipment, cleaned her up and put her in clothes. Bryan took Sophia around the NICU to meet her three siblings, then Dr. Johnson accompanied them outside. The couple stood holding her for about 20 minutes before she took her last breath.

“We were outside the children’s hospital lobby and it was dusk and it started to drizzle,” Amy said, choking back tears. “We went to the church at the top of the hill and prayed for Sophia. We prayed for her to be the others’ angel. I believe she was, because after that, things started to get better.”
The day after Sophia died, Grace needed a four-hour surgery for retinopathy of prematurity, which is a disease that occurs in premature babies that causes abnormal blood vessels to grow in the retina. This growth can cause the retina to detach from the back of the eye, leading to blindness. The surgery went well and saved Grace’s eyesight.
For the next month, the three continued to get bigger and stronger. After more than 100 days in the NICU, the Goodman children, finally started coming home. All three of them needed to have in-home oxygen, apnea monitors and a long list of medications that Amy and Bryan would need to administer at home.
Grace was the first one to come home on April 18.
“That’s my homecoming day, girl,” Grace says with a little bit of adorable sass.
“Yes, that is something we do with all the kids,” Amy explained. “We celebrate their homecoming day, because they have to share their birthday. It’s like a birthday, but it is one-on-one with each of them. They get to pick what they want to do.”
Reece came home April 24, which was close to Amy’s original due date of April 26. Clark needed a little longer stay, but finally was able to come home on May 11.
The NICU social worker was a huge help to the Goodmans helping them with insurance questions and getting them help at home with the kids.
“When they came home I had to give each of them seven to eight syringes a day and organize it with each of their milk intakes. I had a whole pharmacy in my house that I had to be trained on, like how to draw it, how much to draw,” Amy said. “The nurse was coming in the morning, but we quickly realized that we weren’t getting any sleep because their apnea monitors were going off all the time. They weren’t to the point that they were turning blue, but enough that we wanted to check on them. In addition to getting up to feed them at 1 a.m., 4 a.m. and 7 a.m., we weren’t getting any sleep.”
Amy and Bryan hired a nursing student from the local community college to sit with the babies at night to watch their apnea monitors, take care of feedings and change diapers. The student stayed with the family for six weeks until the kids were off of oxygen and the monitors.
“Taking home one 25-weeker is a lot. They go home on oxygen, a monitor and multiple medications. Take that times three and it is just unreal,” Dr. Johnson said. “None of them had to be readmitted after they went home. That, in and of itself, is unbelievable.”
Each kid has had his or her share of hospital stays due to complications from their prematurity, but none have been very serious. Grace has had two more eye surgeries and still visits an eye specialist. Reece has had the fewest effects from his premature birth. He had hernia surgery and tubes placed in his ears.
Clark has been hospitalized every year since he was 3 for difficulty with his lungs. He has asthma and chronic kidney disease that needs to be watched closely, because he could need a transplant in the future. He still sees a lot of specialists for his lungs and kidneys.
“Once Clark was in the hospital for whooping cough,” Amy said. “These kids are great patients — I will say that.”
“Whoop! … Whoop! … Whoop,” the kids chanted like fire engines.
“And always entertaining,” Amy added, laughing.
At 11 years old, the Goodman all have their own personalities and likes.
Reece is quiet and the athletic one. He looks like a mini-version of his father. He loves to play and watch sports, and he wants to be a sportscaster or a professional basketball player.
Clark is the cut-up of the group and likes playing video games, building with Legos and hanging out with friends. He wants to be a sneaker designer or an ice cream tester when he gets older.
Grace is an animal lover. She likes to ride horses and wants to be a dog or horse trainer in the future.
“These kids had reasons to not turn out the way they did. The way they turned out is a testament to not only the care we provide but also the care the parents offered after they took them home,” Dr. Johnson said. “With each of these children, we were looking at a 50-50 chance of survival. To look at these kids now, at 11 years old — it creates a real ‘wow’ moment.”
The Goodmans are very thankful for all the neonatologists and nurses and the care they received in the NICU at Geisinger Janet Weis Children’s Hospital.
“The NICU nurses were fantastic. They were amazing,” Amy said. “When I would ask a question, they were very honest with the answer.”
“We didn’t want for anything. Whatever we needed, they got for us,” Bryan said.
For Bryan and Amy, the miracle is not the kids, but the care that allowed their kids to survive.
“They aren’t miracles. I hate to bust your bubble, but they’re not,” Bryan said with a chuckle as the kids talked over each other, telling jokes and trying to be the center of attention. “I don’t know how someone can be born that early and survive. That’s the miracle of it: the medicine and the care. The miracle is the people who work there and the people who are developing the life-saving stuff.”
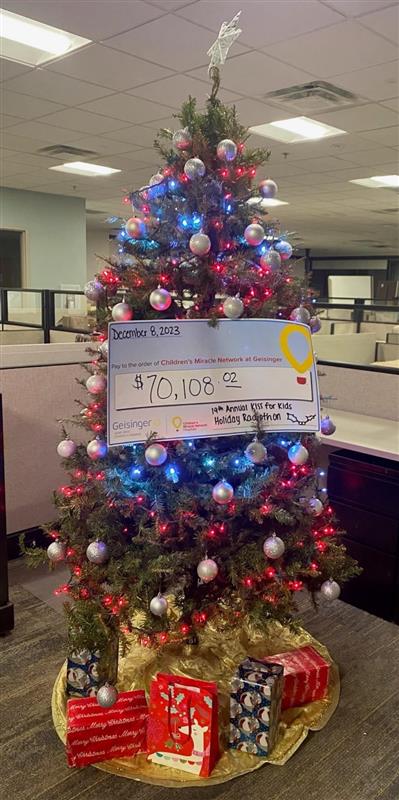
Children’s Miracle Network at Geisinger provided ventilators, monitors, bed warmers, CPAP devices and isolettes for the NICU at Geisinger Janet Weis Children’s Hospital. Children’s Miracle Network routinely upgrades and updates the life-saving equipment used in the NICU for children like the Goodmans.