2016 Miracle Kid Nevaeh Brown

Nevaeh Brown is a quiet, shy little girl, but don’t judge her by her size or timidity. The 3-year-old is as tough as they come, and has been that way since she was born prematurely in May 2013.
A little more than 6 months into her pregnancy, Brenda Hummel began to have issues. During a routine doctor visit, she was told that she had high proteins in her urine and her blood pressure was very high. Her doctor said she may need to deliver.
“It was a big shock,” Brenda said. “I was worried that she wasn’t going to make it or wouldn’t be able to breathe.”
Brenda was sent to Geisinger Medical Center in Danville on April 29 and was monitored. On May 1 things took a turn for the worse.
“While Brenda was here, things got worse and they had to move to deliver the baby emergently,” said Lauren Johnson, MD, neonatologist at Geisinger Janet Weis Children’s Hospital. “The baby was lying breach and they had a lot of trouble getting her out.”
At birth, Nevaeh was not breathing and needed chest compressions to be revived. Soon after, she began breathing on her own, but her battle had just began. She was 26 weeks and 3 days, and she weighed only 1 pound, 7 ounces. For Brenda, who was only 24, the situation was overwhelming and scary. She was happy to have her mother, Barb Crispell, by her side and the caring staff of Geisinger Janet Weis Children’s Hospital’s Neonatal Intensive Care Unit. Nevaeh’s father, Rodney Brown, who needed to work, spent every weekend with Brenda and Nevaeh.
Nevaeh was intubated and put on an oscillator, which is a type of ventilator that keeps the baby’s lungs from being damaged. Things seemed to be moving ahead pretty well. Nevaeh was feeding more and was getting stronger in her first week of life, according to Dr. Johnson.
On day 12, Nevaeh developed a little feeding intolerance, which was felt to be stage 1 necrotizing enterocolitis. Necrotizing enterocolitis is an intestinal disease where the wall of the intestine becomes inflamed allowing bacteria to cause further damage.
“There are different stages. Stage 2 is when you know the baby has it for sure. Stage 3 is when you have to go to the operating room. That’s the inflammatory process in the bowel, and it can get so bad that it can cause perforations and has a 25 percent mortality rate,” Dr. Johnson explained.
Dr. Johnson thought Nevaeh had the mildest form.
“She was at a point where one neonatologist would say she had it and the next would say she didn’t. She was treated like she had it. She didn’t feed and was on antibiotics for a week,” she said.
When she finished the antibiotics and it was time to try to refeed her, Nevaeh could not tolerate her feeds.
“She gave everyone a dickens of a time. We couldn’t feed her. So we thought maybe it was a motility issue, because her gut wasn’t moving appropriately, or maybe it was a formula issue,” Dr. Johnson said. “So we kept taking her down to more elemental formulas. It got to the point that we needed to do a dye study.”
The study was done in the form of a gastrografin enema, which allowed the doctors to see what was going on in Nevaeh’s intestinal tract. The study showed something very uncommon for an infant with the lowest form of necrotizing enterocolitis: a stricture or a narrowing of her colon.
“A stricture is a known complication of necrotizing enterocolitis, but what was weird was that she had the most mild form,” Dr. Johnson said. “Those kids are not the ones that usually get strictures.”
Nevaeh needed surgery to remove the section of the bowel where the stricture was located.
“That is where things kind of fell apart for her,” Dr. Johnson said. “Shortly after the surgery, she developed an abdominal wound infection and an enterococcal infection that was in her bloodstream.”
The infection combined with the necrotizing enterocolitis required Ronald Scorpio, M.D., director of Pediatric Surgery and Pediatric Trauma, to operate a few times.
“Sometimes we remove certain areas that are necrotic and then we have to go back a second time or a third time, and that was the case with Nevaeh,” Dr. Scorpio said.
After the additional surgeries, Nevaeh had a very difficult time recovering. The surgeons couild not close her belly due to excessive swelling. After trying a few different options, they decided to place a special mesh covering over Neavaeh’s belly to help keep her intestines covered and safe.
“When you have an infection, the body tries to fight off the infection. The swelling was an indicator of just how sick she was,” Dr. Scorpio said. “We couldn’t close the abdomen, because that would push up on her lungs. So we put a temporary closure over the belly until the swelling resolved itself and we could close the belly.”
Nevaeh had seven surgeries on her intestines while she was in the NICU, she also needed several blood transfusions and antibiotic treatments, as well as breathing assistance.
She also had scarring of her retina, which can cause blindness. Doctors gave Nevaeh an injection of Avastin to help save her vision.
“She was on the ventilator and every time they would take it off, she would have another surgery and she would have to be put back on,” Brenda said. “She would be doing well one minute and the next minute her breathing would go downhill.”
After one of the operations, Nevaeh’s intestines leaked into her bowel space. She developed peritonitis, which is inflammation of the peritoneum, or the membrane lining the inner abdominal wall and covering the organs in the abdomen.
“She had four really big antimicrobials for a total of 14 days. Those are all things that keep stacking up — the long respiratory course, the necrotizing enterocolitis, the infections and all the operative interventions,” said Dr. Johnson. “There were some times during her course, that is was very touch-and-go for Nevaeh.”
Brenda and Barb stayed in the NICU as long as they possibly could each day but would go to a local hotel at night to sleep and freshen up. One night, they received a call in the middle of the night asking them to get to the hospital immediately. Rodney rushed to Danville to be by their side.
“We got there and everyone in the NICU stopped doing what they were doing and followed us to Nevaeh’s bed,” Barb said. “I turned around and saw the staff following us to her bed, and I felt like this was it. She wasn’t going to make it.”
Nevaeh had reached a critical point where the staff was not sure if she would make it. But her strength and determination, along with the help of the NICU staff, helped to pull her through. The swelling went down and slowly Nevaeh was able to overcome the infections and breathing issues.
After an almost four-month stay in the NICU, Neveah was able to go home with her mother on Aug. 20. She was sent home with a colostomy bag and her abdominal wall was still open. The staff and Phoebe Beckley, NICU March of Dimes family support specialist, taught Brenda how to care for Nevaeh.
“Barb and Brenda both came to our programs and activities,” Beckley said. “They were very active, and I think they were important in encouraging the other families. They would get other people to participate and provided a lot of support to the other families.”
Brenda and Barb took advantage of pastoral care offered by the NICU Pastor Jasmine Loney.
“I spent a lot of time with Nevaeh’s family and had a close relationship with them,” Loney said. “Most times, it is just listening to them and offering them anything they needed. They asked if I would baptize Nevaeh while she was in the hospital, so I created a baptism ceremony specifically for their family.”
“Jasmine was wonderful. Every time she came in, she prayed with us and she always came to see Nevaeh,” Brenda said.
After Nevaeh had time to grow and heal at home, she went back for one more surgery to reconnect her bowel. Since then, she has not had to go back to the hospital.
“The care at Geisinger is amazing. The nurses were great. The doctors were great. There is no other hospital we would ever go to now,” Brenda said. “I have a friend who recently had her baby, and she was in the NICU in Danville. I told them, ‘It is the best place you can be. I love it down there.’”
Rodney shares Brenda’s beliefs about Geisinger Janet Weis Children’s Hospital.
“It is the best hospital around,” he said. “I am so that they took such great care of Nevaeh.”
She is followed by Lela Brink, MD, pediatrician at Geisinger Gray’s Woods in State College.
“I have taken care of Nevaeh since she got out of the hospital,” Dr. Brink said. “She had her colostomy removed in January 2015 when she was a year and half old. Since then, she has been doing great. Developmentally, she just took off. She is growing on the normal growth curve.”
Nevaeh also saw Dr. Scorpio and gastroenterology specialists at Geisinger Gray’s Woods multispecialty clinic, which was very convenient for the family and saved them from traveling to Danville for visits.
Nevaeh turned 3 in May and has been doing extremely well, according to Brenda.
“Her learning skills are great. Things that we were worried that she may be delayed on, she is not,” Brenda said, as Nevaeh fell on her face running across the room. “She’s tough. There are times when she has ear infections and we don’t even know. Dr. Brink will ask, ‘She wasn’t pulling her ears?’ I think she is used to the pain.”
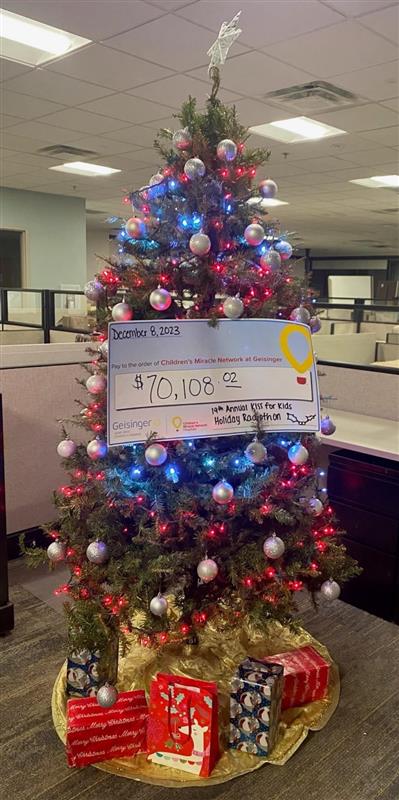
Dr. Johnson is very thankful for donations to Children’s Miracle Network at Geisinger that help in the care of patients like Nevaeh.
“Neonatology is always evolving, and Children’s Miracle Network funds allow us to evolve as rapidly as we can so that we are not sitting here saying we need donor breast milk or humidfied isolettes,” she said of two items recently paid for with donations. “We just bought a bunch of theses isolettes, but our originals were bought through donations. It allows us to get these items and show how they make a difference in our patients’ care.”
As for Nevaeh, she is happy to be watching Doc McStuffins, Elmo and Barney or playing with her cousins Zoey, Julia and Cooper.
“One thing about Nevaeh is she is a very strong baby, because how she made it, I do not know,” Barb said.
Dr. Brink couldn’t be happier with Nevaeh’s progress and credits her family for their hard work in her care.
“She is only here now for her well visits and is a normal kid,” Dr. Brink said. “She is a miracle because she was a teeny-tiny preemie, and she tolerated all the surgery and problems with her bowel really well. The second thing is, she has great family support and they were able to care for her when she came home with her bowel issues. She is growing up and developing very well.
Dr. Scorpio said it is easy to see why Nevaeh is a miracle.
“She was so small and so sick — and she’s alive.”
Donations to Children’s Miracle Network at Geisinger provided ventilators, isolettes, monitors, warmer beds and many more items in the Neonatal Intensive Care Unit that were used in Nevaeh’s care. The Neonatal Pastoral Care position was created with Children’s Miracle Network funds.